Laparoscopic Nephroureterectomy
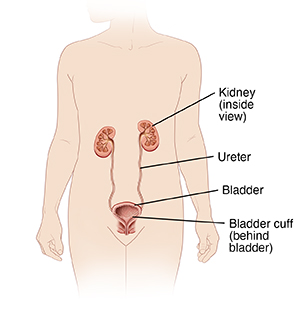
Laparoscopic nephroureterectomy is surgery to remove a kidney and ureter. You may need this surgery for cancer in a kidney or ureter. Your two kidneys are organs that filter your blood. They remove waste chemicals and extra water to make urine. Ureters are tubes that carry urine from your kidneys to your bladder.
For the surgery, the surgeon uses a tool called a laparoscope (scope). This is a thin, lighted tube with a camera on the end. The scope lets the surgeon work through a few small cuts (incisions). In most cases, after surgery your body can still work well with only one healthy kidney and ureter.
How to say it
LA-puh-reh-SKOP-ihk
NEHF-roh-YOOR-ee-tuhr-EHK-tuh-mee
Getting ready for surgery
Follow any instructions from your healthcare provider.
Tell your provider about any medicines you are taking. You may need to stop taking all or some of these before the test. These may include:
-
All prescription medicines
-
Blood-thinning medicines (anticoagulants)
-
Over-the-counter medicines such as aspirin or ibuprofen
-
Street drugs
-
Herbs, vitamins, and other supplements
In addition:
-
Don't eat or drink during the 8 hours before your surgery. This includes coffee, water, gum, and mints. If your healthcare provider tells you to take medicines, take them with a small sip of water.
-
Get your bowel ready for surgery 1 to 2 days before the surgery, if you have been told to. You may need to limit your diet to only clear liquids. You may also be asked to take laxatives or to give yourself an enema. Follow your healthcare provider’s instructions.
The day of surgery
The surgery usually takes 3 to 5 hours. After surgery, you will usually stay in the hospital for 1 to 3 nights.
Before the surgery begins
-
An IV (intravenous) line is put into a vein in your arm or hand. This line supplies fluids and medicines such as antibiotics.
-
You may be given medicine to prevent blood clots.
-
To keep you free of pain during the surgery, you are given general anesthesia. This medicine puts you into a deep, sleeplike state through the surgery. A tube may be put into your throat to help you breathe.
During the surgery
-
The provider makes a few small incisions and one slightly larger incision in your belly (abdomen).
-
The provider puts the scope through an incision. The scope sends live pictures of the inside of your abdomen to a video screen.
-
The provider fills your abdomen with gas. This makes space for the provider to better see and do the surgery.
-
Using tools placed through the incisions, the provider prepares the kidney and ureter for removal. The provider detaches the small piece of tissue where the ureter connects to the bladder (bladder cuff).
-
The provider removes the kidney, ureter, and bladder cuff through the larger incision. Nearby lymph nodes may be removed as well.
-
When the surgery is complete, the provider removes all of the tools. They close the incisions with stitches or staples.
-
The provider puts a thin tube (Foley catheter) in your bladder. This will drain your urine while your bladder heals.
The provider will often begin with laparoscopy. But the procedure may need to change to open surgery for safety reasons. Open surgery is done using a larger incision in your abdomen or side. You’ll be told more about this possibility before surgery.
Recovering in the hospital
After the surgery, you will be taken to the PACU (post anesthesia care unit). There, you’ll be closely monitored as you wake up from the anesthesia. You may feel sleepy. You may have an upset stomach (nausea). If a breathing tube was used, your throat may be sore at first. When you are awake and stable, you will be taken to your hospital room. While in the hospital:
-
You will be given medicines to manage your pain, as needed. Let your provider know if your pain is not going away.
-
You’ll first get IV fluids only. In a day or so, you’ll start on a liquid diet. You’ll then slowly return to a normal diet.
-
You’ll be taught ways to cough and breathe that can keep your lungs clear and prevent pneumonia.
-
The healthcare team may remove the Foley catheter while you’re in the hospital. If not, you’ll be taught how to care for it at home.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days to help care for you. Recovery time varies for each person. Your provider will tell you when you can return to your normal routine. Until then, follow the instructions you have been given. Make sure to:
-
Take all medicines as directed. Consider using a pill tray or electronic reminders so you don't miss any doses.
-
Care for your incisions and catheter as instructed.
-
Follow your provider’s guidelines for showering. Don't swim, bathe, use a hot tub, or do other activities that cover the incision with water until your provider says it’s OK.
-
Don't lift anything heavy or do strenuous activities, as directed by your provider.
-
Don't drive until your provider says it’s OK. Don't drive if you’re taking medicines that make you drowsy or sleepy.
-
Walk at least a few times a day. Increase your pace and distance, as you feel able.
-
Don't strain to pass stool. If needed, take stool softeners as directed by your provider.
-
Drink plenty of water. This helps prevent urine odor and dehydration. Follow any special diet instructions from your provider.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Chest pain or trouble breathing ( call 911 )
-
Fever of 100.4° F ( 38°C) or higher, or as directed by your healthcare provider
-
Symptoms of infection at incision site—these include increased redness or swelling, warmth, more pain, or bad-smelling drainage
-
Bloody urine or drainage from the catheter that is dark red or has clots (a small amount of blood is normal)
-
No drainage from the catheter for more than 4 hours
-
The catheter comes out of your bladder
-
Pain that can't be controlled with medicines
-
Pain or swelling in your legs
-
New or worsening symptoms
Follow-up
You’ll have follow-up visits so your provider can check how well you’re healing. If your stitches, staples, or catheter need to be removed, this will likely be done in 7 days. During follow-up visits, you may need tests to make sure the cancer has not returned. Keep all of your follow-up appointments. Consider bringing a close family member or friend to your appointments to be certain all of your concerns are addressed.
Risks and possible complications
All procedures have some risk. The risks of laparoscopic nephroureterectomy include:
-
Bleeding (may require a blood transfusion)
-
Infection
-
Blood clots
-
Hernia at the incision sites
-
Damage to nearby nerves, blood vessels, soft tissues, or organs
-
Cancer returning or tumor seeding (spillage of tumor cells that can grow into new tumors)
-
Problems with the remaining kidney. This could lead to kidney failure.
-
Heart attack or stroke
-
Risks of anesthesia. The anesthesiologist will discuss these with you.