Ependymoma
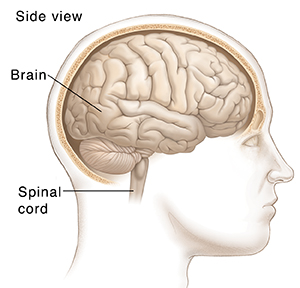
Ependymoma is a rare type of tumor that starts in the brain or spinal cord. It can occur in both children and adults. It's more common in childhood, when it starts in the brain. In adults, these tumors most often start in the spinal cord.
An ependymoma may not be cancer (benign), or it may be cancer (malignant). A malignant ependymoma can spread. A benign one can't. Both types can cause problems as they grow and press on nearby tissues.
How does an ependymoma grow?
Your brain and your spinal cord make up your central nervous system (CNS). Ependymoma is a primary CNS tumor. This means it starts in the tissues of the brain or spinal cord instead of starting in another part of the body and spreading to the CNS. Even small CNS tumors can cause problems by pressing against nearby nerves and tissues.
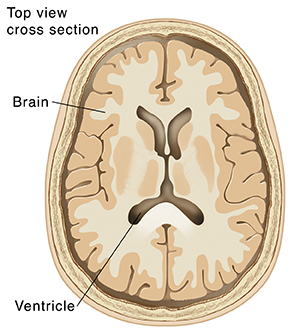
Ependymoma is a kind of glioma. It starts in the glial cells. These cells support the CNS. The tumor is caused by out-of-control growth of ependymal cells, which are a type of glial cell. These cells line fluid-filled chambers of the brain called ventricles. The ventricles contain the cerebrospinal fluid (CSF). This is the fluid that surrounds and protects the brain and spinal cord. The cancer cells can get into the CSF and spread to other places in the brain or spinal cord. These tumors rarely spread beyond the CNS to other parts of the body.
Ependymomas are grouped by how big the cells are, what shape they are, how fast they grow, and where they are. They are also grouped by the tumor size, consistency, and spread.
There are 5 types of ependymoma tumors:
-
Subependymoma (Grade I). This type is a benign (not cancer) tumor in the ventricles. It often grows slowly.
-
Myxopapillary ependymoma (Grade I). This tumor is slow growing. It tends to start at the bottom of the spinal cord.
-
Classic (conventional) ependymoma (Grade II). This type is most common. It grows a bit faster.
-
RELA fusion-positive ependymoma (Grade II or III with a change in the RELA gene). These tend to be more common in children.
-
Anaplastic ependymoma (Grade III). This tumor is often near the base of the brain. It grows faster than the other types.
What causes an ependymoma?
Researchers don't yet know what causes these tumors. The risk factors for these kinds of tumors aren’t known. There's no known way to prevent them.
What are the symptoms of an ependymoma?
Symptoms can vary from person to person. They depend on where the tumor is. For instance, a tumor near the base of the brain may block the normal flow of CSF. This can increase the pressure in your skull and cause headaches, nausea, vomiting, and dizziness.
Your symptoms may be sudden. Or they may start slowly and get worse over time. In general, signs and symptoms of ependymoma can include:
-
Headache
-
Nausea and vomiting
-
Dizziness and balance problems
-
Eye problems, such as double or blurry vision
-
Weakness or numbness in an arm or leg
-
Trouble walking
-
Bowel or bladder problems
-
Back pain that spreads to the arms or legs
How is an ependymoma diagnosed?
Ependymoma can be hard to diagnose. It's a rare tumor in adults. And it may be hard to tell the difference from other types of tumors. Your healthcare provider may refer you to a neurologist. This is a healthcare provider who specializes in diseases of the CNS. You may also see a neuro-oncologist. This healthcare provider specializes in treating cancers of the brain and spinal cord. Or you may be referred to a neurosurgeon. This is a surgeon who operates on the brain or spinal cord.
The process starts with a medical history and a physical exam. Your healthcare provider will ask about your symptoms and past health. You may also be asked about your family’s medical history.
The physical exam may include a neurologic exam. During this exam, your healthcare provider may ask you to do things like walk, touch your finger to your nose, follow a light with your eyes, or hold your hands out.
You may also need tests such as:
-
MRI (magnetic resonance imaging). This scan uses magnets and a computer to make detailed images of the inside of your body. MRI scans of your brain and spinal cord are used to get more information about the tumor. Contrast dye may be used to help show clearer details.
-
Lumbar puncture. This test is also called a spinal tap. A thin needle is put between the bones in your lower back. It's used to take out a small amount of CSF from the space around your spine. The fluid is checked for tumor cells.
-
Biopsy. This test is often needed to diagnose an ependymoma. It's when a piece of tissue or fluid (called a sample) is tested for cancer cells. The biopsy is often done during surgery to take out a small piece of the tumor or try to remove the tumor. The removed tissue is tested in a lab to learn more about the tumor.
How is an ependymoma treated?
Your healthcare team will work with you to make a treatment plan. Your team may include:
Treatment depends on what type of tumor it is and where it is. The main treatment is surgery. This is done to remove as much of the tumor as possible. Tests will be done on the tumor to find out more about it.
You may need radiation therapy or chemotherapy after surgery. Radiation therapy is done by sending beams of energy to the site of the cancer. Chemotherapy is used less often. It's done with strong medicines that kill cancer cells. They may be given by mouth, IV, or injected into your spinal fluid (intrathecal).
Follow-up care
You will be watched closely after treatment. Sometimes, ependymomas come back (recur) after treatment. Your provider will watch for this, as well as long-term treatment side effects. You'll likely need to have follow-up MRI scans every 3 or 4 months for the first year, and then a few times a year after that.