Peptic Ulcer
A peptic ulcer is a sore in the lining of your stomach or in the first part of your small intestine (duodenum). It can cause belly (abdominal) pain and other symptoms. In some cases, a peptic ulcer may get worse. This can lead to serious problems such as bleeding, a hole (perforation), or a blockage (obstruction) in the stomach or duodenum. Treatment is needed to prevent these complications. With treatment, most people fully recover.
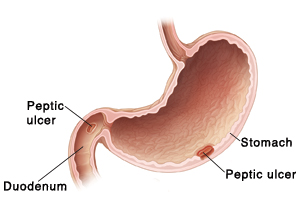 |
| Peptic ulcers can occur in the stomach or duodenum. |
Common causes of a peptic ulcer
A peptic ulcer can be caused by:
-
Infection from H. pylori (Helicobacter pylori) bacteria
-
Long-term use of pain medicines called nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, naproxen, and ibuprofen
-
Physical stress, such as burns, head injuries, needing a breathing tube, or being on blood-thinning medicine
-
Other rare causes
How a peptic ulcer forms
The lining of your stomach and duodenum is coated with a thick mucus layer. This helps protect the stomach and duodenum from the acids and enzymes they make to help break down the food you eat. When H. pylori is present, it can weaken the mucus layer and irritate the lining underneath. Acid may pass through the weakened mucus layer and cause an ulcer to form. Overuse of NSAIDs can also damage the mucus layer, leading to ulcers.
Symptoms of a peptic ulcer
Peptic ulcers may or may not cause symptoms. If you do have symptoms, they may come and go. They may also range from mild to severe. Common symptoms include:
-
Burning feeling, cramping, or hunger-like pain in the stomach area (often 1 to 3 hours after a meal, or in the middle of the night)
-
Pain that gets better or worse with eating
-
Loss of appetite
-
Weight loss
-
Nausea or vomiting (vomit may be bloody or look like coffee grounds)
-
Black, tarry, or bloody stools (this means the ulcer is bleeding)
Diagnosing a peptic ulcer
Your healthcare provider will ask about your symptoms and health history. You’ll also have a physical exam. In addition, tests will be done to confirm the problem. These tests also help find out if an ulcer is caused by H. pylori. Tests can include:
-
Blood, stool, or breath tests. These are done to check for H. pylori and other problems. For blood and stool tests, small samples of your blood and stool are taken. The samples are sent to a lab to be looked at. For a breath test, you'll drink a liquid that contains a harmless compound. H pylori causes the compound to break down and release carbon dioxide gas. By testing the air you breathe out after you drink the liquid, the healthcare provider can tell if the bacteria are present.
-
Upper endoscopy. This test is done to see inside the stomach and duodenum. This lets your healthcare provider check for ulcers. During the test, an endoscope (scope) is used. This is a thin, flexible tube with a tiny camera on the end. Once you are given sedation for comfort, the scope is inserted through your mouth. It's then guided down into your stomach or duodenum. If needed, tiny tools may be passed through the scope to take tissue samples (biopsy). Treatment can also be done at the same time if bleeding or other problems are found.
-
Upper gastrointestinal (GI) series. This test is done to take X-rays of your upper digestive tract from your mouth to the small intestine. This lets your provider check for ulcers. For this test, you’ll drink a milky liquid that has a substance called barium. The barium coats your upper digestive tract so that it will show up clearly on X-rays.
Treating a peptic ulcer
Medicines are the most common treatment for peptic ulcers. They include:
-
Antibiotics. These will treat the H. pylori bacterial infection. In many cases, you’ll need to take at least 2 types of antibiotics.
-
Proton pump inhibitors. These block your stomach from making any acid.
-
H2 blockers. These reduce the amount of acid your stomach makes.
-
Bismuth subsalicylate. This helps protect the lining of your stomach and duodenum from acid.
Take all of the medicines that you’re prescribed exactly as instructed. Don’t stop taking the medicines, even if you're feeling better. The medicines may cause side effects. Your healthcare provider will tell you more about these based on which medicines you're prescribed. During treatment, don't take aspirin and other NSAIDs. You may also be told to stay away from cigarettes, alcohol, and caffeine. These may make your symptoms worse or affect how well your ulcer heals. If your stress level is high, reducing stress may help.
In severe cases, other treatments will likely be done. These may include procedures with an endoscope or surgery. Your provider will tell you more about these treatments, if needed.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Chills
-
Frequent vomiting, blood in your vomit, or coffee ground-like substance in your vomit
-
Sudden or severe belly pain
-
Dark, tarry, or bloody stools
-
Weight loss
-
Pain that doesn't get better, even with treatment
Preventing a peptic ulcer
Take the following steps to help prevent a peptic ulcer:
-
Reduce your risk for H. pylori infection. Most experts think that H. pylori can be passed through food or water that's contaminated by an infected person. For your safety, the CDC advises following basic hygiene. For instance, always wash your hands with clean, running water and soap after using the bathroom. Wash your hands before making and handling food. Only drink water from safe sources.
-
Limit the use of aspirin and NSAIDs. Work with your healthcare provider to change your medicine or to reduce the amount of NSAIDs you take. If you must take aspirin or NSAIDs, ask your provider about other pain medicines you can take to help protect your stomach and duodenum. Sometimes other pain medicines can be used instead. But if you take aspirin because of a heart condition, blood clot, or stroke, talk with your healthcare provider first before you stop taking aspirin.
-
Quit smoking. Quit other forms of tobacco, too.